I-InTERACT-North: Examining a virtual mental health stepped care approach to addressing needs of at-risk children and families

At a glance
Issue
“Families of children with medical complexities had psychosocial and early intervention needs that were not being met by existing community programs. These families expressed that community providers felt their needs were too complex and they were left with little to no support. Parent advocacy for support in this area eventually led to team efforts to understand where services and research could be provided to help address these concerns…. leading to the I-InTERACT-North program.” - I-InTERACT-North Therapist, R. Lyon
Research
With CIHR funding, a team of researchers, health care providers, and family leaders are embedding implementation science and equity, diversity, and inclusion approaches to develop and implement a transdiagnostic and evidence-based virtual parenting program. This program supports families of children with diverse neurological, cardiac and neurodevelopmental diagnoses.
Impact
Children and families who participate in the I-InTERACT-North program experience meaningful health and social benefits. The program continues to extend its reach to serve more children and families as the research team continues to identify and address key facilitators and barriers to implementation. By being involved with the program, research team members and clinical partners are also further developing their professional capacity.
The following case study was contributed by:
- Tricia Williams (Department of Psychology, Division of Neurology, The Hospital for Sick Children, Toronto ON)
- Rachel Lyon (Department of Psychology, The Hospital for Sick Children, Toronto ON, Department of Psychology, York University, Toronto ON, LaMarsh Centre for Child and Youth Research, York University, Toronto ON)
- Marin Taylor (The Hospital for Sick Children, Toronto ON)
- Juanita Atton (The Hospital for Sick Children, Toronto ON)
- Rivka Green (Department of Psychology, The Hospital for Sick Children, Toronto ON)
with support from the team at the CIHR Institute of Human Development, Child and Youth Health.
I-InTERACT-North is an evidence-based virtual parenting program for families of children with developmental challenges stemming from early brain injury. The program emphasizes positive parenting techniques to establish guidelines for behaviour management. Teaching families how to build positive and responsive relationships to address challenging behaviours has been shown to be effective at reducing mental health and behavioural problems. This improves family dynamics and reduces parental stress. Community-based resources during the COVID-19 pandemic were less available, and families of children with neurodevelopmental challenges struggled to find necessary supports. These families were thus at a heightened risk of significant mental health consequences. With CIHR support, our team implemented a stepped care model of the program (‘Stepping Up to COVID’ (Study name))— at The Hospital for Sick Children in Toronto. This offered an effective and tailored treatment approach that adapted to families’ fluctuating needs, making it easier to follow the program and stick with it. The second COVID-19 CIHR-funded study builds on this previously implemented stepped-care version of the I-InTERACT-North program, extending it within multiple programs at SickKids and among children and families in the Province of Ontario Neurodevelopmental Disorders Network (POND). We used a mixed-method design to meet the project objectives: 1) evaluation of the effectiveness and acceptability of the program, and 2) identification of participant and care provider perceptions of the program to help inform future trials.
Key benefits of the I-InTERACT-North research program

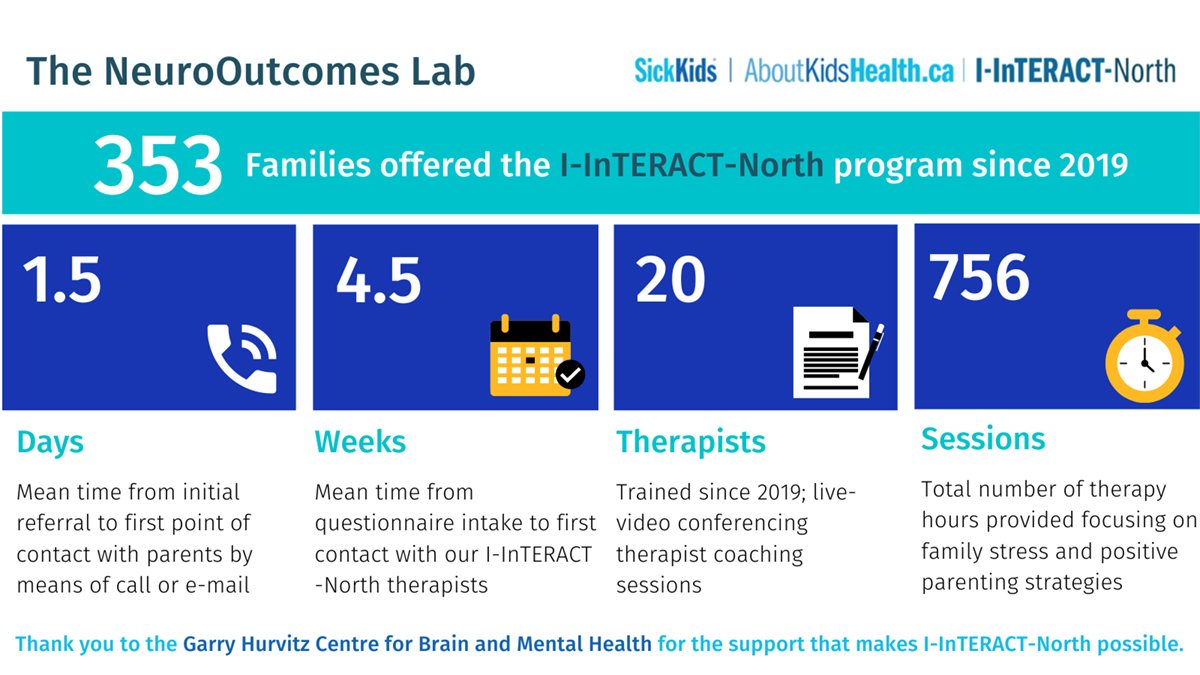
Clinical Impact: The expansion of the I-InTERACT-North program to include additional at-risk populations—including, but not limited to, neurological, cardiac and neurodevelopmental diagnoses— in addition to its online delivery, has enabled it to reach an extensive at-risk pediatric population across Ontario (see Figure 1).
The CIHR-funded project opened the program up to include kids without medical conditions but who nonetheless presented as at risk for behavioural issues due to neurodevelopmental profile (e.g. ASD, ADD/ADHD, OCD, LD). This was largely due to a new collaboration with the Province of Ontario Neurodevelopmental (POND) Network.
With this CIHR funding we transitioned from a one-size fits all to a stepped-care approach as informed by the Choice and Partnership Approach (York 2009) to enhance service effectiveness and family satisfaction. This directly improved patient acceptability, recruitment, and retention (Deotto 2023).
Future impact now extends to a clinical implementation trial, transitioning I-InTERACT-North into routine care at SickKids. Over the next three years, we have funding to work towards our goal of transitioning I-InTERACT-North from a research-funded intervention into part of usual clinical care for children and families across several clinics at SickKids (Neonatal, Cardiology, Neurology, Psychiatry and Genetics). We will be following the Implementation Roadmap (Barwick 2023) to help maximize the program’s sustainability by determining how I-InTERACT-North meets clinician and partners’ needs, preparing informed clinical service pathways for installation, and determining initial experiences of its implementation into standard of care.
Long Description
The NeuroOutcomes Lab
| 353 Families offered the I-InTERACT North program since 2019 | |||
| 1.5 | 4.5 | 20 | 756 |
| Days | Weeks | Therapists | Sessions |
| Mean time from initial referral to first point of contact with parents by means of call or e-mail | Mean time from questionnaire intake to first contact with our I-InTERACT-North therapists | Trained since 2019; live-video conferencing therapist coaching sessions | Total number of therapy hours provided focusing on family stress and positive parenting strategies |
| Thank you to the Garry Hurvitz Centre for Brain and Mental Health for the support that makes I-InTERACT-North possible. | |||
Highlighting the expertise underlying the research program
“The program itself was designed by a psychologist and implemented by a neuropsychologist, which speaks to the level of research-based evidence behind the foundations of the program. Furthermore, all who have been/are involved in the program delivery are trained in that area of neuropsychology.” - I-InTERACT-North Therapist, R. Lyon
Background evidence highlighting program needs. Mental health and neurodevelopmental disorders in children are rising in Ontario. One in every five children is affected by a mental health condition, such as anxiety and depression, and one in every six children is affected by a neurodevelopmental disorder, such as ADHD or autism. In our team’s early work, we established that among children seen at SickKids, with co-occurring medical conditions, up to 50% of children with early brain injury and associated medical conditions are at risk of mental health and neurodevelopmental disorders. In addition to stressors on the family, these mental health challenges are currently not adequately addressed by the education and healthcare systems. In Ontario, there are identified gaps in mental health service and acute needs due to the COVID-19 pandemic and its aftermath. Currently, there is no clinically offered supportive parenting intervention for very young children with early medical conditions at SickKids.
Program impact in community. Knowledge translation and dissemination expertise “skills such as public speaking, good communication, collaboration, passion for community engagement- all of which are needed for delivering presentations at conferences/ grand rounds/ writing manuscripts” have been integral in the project’s impact.” - I-InTERACT-North Therapist, R. Lyon
Unique features of the program such as its virtual delivery and transdiagnostic approach for behaviour management have “positioned us very well to expand and seamlessly provide care to a wide range of families” and thus have played a role in its success. More specifically, the capacity for the team to deliver the program remotely (predating pandemic restrictions) allowed therapists to match the intensity of the services provided to meet the unique needs of each family, thereby allowing the program to align more closely with hospital goals for precision-based care for patients.
The program’s ongoing efforts are informed with EDI principles by “deliberately asking questions about race, religion and values about parenting” and being “responsive to these by adapting program in a way that feels best for families.” - I-InTERACT-North Therapist, R. Lyon
Patient/Family Engagement from the Outset. To align with hospital efforts in providing responsive care, our team has had an active Family Advisory Council (FAC) throughout this project. The FAC consists of parents and caregivers of children who are patients at SickKids and who are interested in providing input and ways to improve this and other current research projects at the lab. FAC meetings occur monthly and aim to provide parents with peer support and an opportunity to engage in the development and improvement of participant-facing materials (ex. I-InTERACT-North module videos, surveys and questionnaire wording, etc.). Feedback gathered from these meetings has been integral to the program development and delivery.
Understanding the details of the impact
Nature of impact - At the child and family level, the program has seen improved child behaviour and family functioning in addition to high acceptability. This is all attributed to the program’s capacity to be adapted to a family’s unique needs and we’ve received some wonderful feedback including comments like this one:
“We really appreciated the program’s flexibility and suggestions for our unique family situation.” - I-InTERACT-North parent participant
At a clinical service level, clinicians report high relevance of the program as a referral source:
“I am so pleased to be able to refer our patients to the I-Interact-North program, given the program targets symptoms that typically occur in diagnoses that we do not provide targeted mental health treatment for in [referring department] (e.g., ADHD/disruptive behavioural disorders). As well, the program incorporates treatment modalities not offered within the department.” - Clinical partner – referral
In terms of professional capacity building, the program has provided an opportunity for early career mental health professionals to receive training and mentorship in an evidenced based virtual mental health intervention:
“All [I-InTERACT-North] therapists have excellent training and research background in mental health and are able to provide the necessary psychoeducational therapy required in the program. The therapists involved have comprehensive educational background and are knowledgeable about neurodevelopmental conditions and their behavioural manifestations.” - I-InTERACT-North therapist, R. Lyon
Reach - To date the program has been offered to over 300 families across Ontario. Parents reported that the program and their assigned therapist incorporated their family’s cultural or racial heritage to guide treatment. Future reach and equity, diversity and inclusion (EDI) opportunities for larger scale implementation include hybrid in-person/virtual formats, knowledge dissemination across rural and urban settings, translations of program materials to various languages, and expanding racial, cultural, and neurodiverse identity representation in program video content.
Sustainability – Parents and clinical partners identified key facilitators and barriers to inform the scale and spread of the program, and 2) equity, diversity, and inclusion considerations to be integrated in future clinical implementation. Positive perceptions of the program’s relevance were echoed across focus groups, with several explicit steps recommended for the program’s clinical implementation. Prominent themes surrounded knowledge dissemination, community building, expansion of program reach, and EDI promotion. Clinical partners provided implementation facilitation recommendations within both inner acute care and outer community settings with respect to system mapping and funding structures.
Stakeholders & Beneficiaries: Children, parents, clinicians, and community service providers have been stakeholders in this program as well as benefiting from the program.
Collecting the evidence for research impact
Data Sources: Several publications (published and under review) provide key quantitative impact data on metrics of the program’s feasibility, acceptability, and clinical impact.
Interviews: An impact interview was conducted with Rachael Lyon, MA. Ms. Lyon is a clinical partner and I-InTERACT-North therapist, program trainer and supervisor. All I-InTERACT-North therapists were also surveyed.
Focus Groups: Between 2022-2023, three focus groups were conducted among key knowledge users (e.g., parents/caregivers, N = 11) and clinical partners (e.g., senior mental health administrative leaders/clinicians, N = 15). We recruited participants for whom the intervention had direct relevance to best inform readiness for program implementation and co-design necessary adaptations for larger scale clinical implementation efforts. Using The Implementation Roadmap (TIR) (Barwick et al., 2023), focus groups examined the perspectives of the I-InTERACT-North program among parents/caregivers and clinical partners for the purposes of identifying: 1) facilitators and barriers to inform the scale and spread of the program, and 2) equity, diversity, and inclusion considerations to be integrated in future clinical implementation.
The role of knowledge mobilization activities in contributing to the impact
Our knowledge-to-action approach involved families, clinicians, scientists, and knowledge users (parents of children with early brain injury and neurodevelopmental disorders) throughout this project. We used integrative and end-of-study knowledge translation approaches.
Integrated and end-of-study knowledge translation (KT) efforts were informed in collaboration with our Family Advisory Group, considering innovative ways of disseminating results including social media graphics, program videos, podcasts, as well as provincial, national, and international webinars and symposia (e.g., Preemie Chats Live Webinar, Children’s Healthcare Canada-SPARK live conversations webinar, Cardiac Neurodevelopmental Outcome Collaborative (CNOC) webinar, International Neuropsychological Society, International Paediatric Brain Injury Society). Individual family advisors were directly involved in several specific iKT activities (e.g., Parenting Podcasts, HIE Peer-to-Peer mentorship webinar) as well as acting as authors and collaborators on publications and new grant applications.
Students and trainees were integral to iKT activities and actively engaged throughout the project, presenting ten posters at national and international conferences and leading/co-authoring seven papers.
Most recently, our group presented at the Children’s Mental Health Ontario (CMHO) annual conference on Early Interventions: Improving Access and Treatment for Infants and Early Years. For this, we partnered with colleagues from the Children’s Hospital of Eastern Ontario. Our specific presentation, Promoting Resilience in Childhood through Innovative Parenting Interventions, highlighted the growing need across the province for working across sectors and hospital sites to create more seamless pathways to earlier mental health care. Additionally, in collaboration with CMHO, we prepared a Call-to-Action for distribution at events to further project impact and raise awareness of the importance of early intervention with quotes from Canadian leaders in pediatric health:
“Access to evidence-based mental health services is essential to improving outcomes for children and youth. I-InTERACT-North is designed to help narrow an important gap in our healthcare system by bringing clinicians and families together sooner to identify and respond to child mental health needs.” - Dr. Ronald Cohn, President and CEO of SickKids
“I-InTERACT-North is an easily accessible and well-suited parenting intervention for families with children with neurodevelopmental disorders, like ADHD or autism, as well as children with behavioural concerns. I-InTERACT-North takes a proactive approach; offering services early on to families with the hope of preventing worsening mental health and behavioural needs later in childhood.” - Dr. Evdokia Anagnostou, Vice President of Research and Director, Bloorview Research Institute
“The I-InTERACT-North program provides a critical opportunity to support parents - and in doing so, improve the mental health outcomes of children cared for in our intensive care unit. The program addresses a need expressed consistently by parents.” - Dr. Steven P. Miller, Professor and Head, Pediatrics, University of British Columbia
Further reading
- Barwick, M., Brown, J., Petricca, K., Stevens, B., Powell, B. J., Jaouich, A., Shakespeare, J. & Seto, E. (2003). The Implementation Playbook: study protocol for the development and feasibility evaluation of a digital tool for effective implementation of evidence-based innovations. Implement Sci Commun, 4(1):21.
- Deotto, A., Fabiano, G. F., Chung, B. Y. T., Wade, S. L., Anagnostou, E., Crosbie, J., Kelley, E., Nicolson, R., Andrade, B. F., Miller, S. P., & Williams, T. S. (2023). Stepping up to COVID-19: A clinical trial of a telepsychology positive parenting program targeting behavior problems in children with neurological risk. Journal of Pediatric Psychology, 48 (6), 523-536.
- Ford, M. K., Roberts, S. D., Andrade, B. F., Desrocher, M., Wade, S. L., Kohut, S. A., & Williams, T. S. (2022). Building I-INTERACT-North: Participatory action research design of an online transdiagnostic parent–child interaction therapy program to optimize congenital and neurodevelopmental risk. Journal of Clinical Psychology in Medical Settings, 30(1), 204–215.
- Wade, S. L., Gies, L. M., Adlam, A. R., Bardoni, A., Corti, C., Jones, K. M., Limond, J., & Williams, T. S. (2023). Pediatric Rehabilitation. In B. Crosson, K. Y. Haaland, T. Z. King, & G. G. Brown (Eds.), American Psychological Association Handbook of Neuropsychology, Vol 1 (pp. 529-553). Washington, DC: American Psychological Association.
- Williams, T. (2021). Transdiagnostic approaches to early brain injury: Harnessing neuroprotection through parents and families: Introduction to the Special Edition. The Clinical Neuropsychologist, 35(5), 841-845.
- Williams, T. S., Burek, B., Deotto, A., Ford, M. K., Green, R., & Wade, S. L. (2022). Pandemic perils and promise: Implementation of a hospital-based virtual parenting intervention during COVID-19. Developmental Neurorehabilitation, 25(8), 505–517.
- Williams, T. S., Deotto, A., Roberts, S. D., Ford, M. K., Desire, N., & Cunningham, S. (2022). COVID-19 mental health impact among children with early brain injury and associated conditions. Child Neuropsychology, 28(5), 627-648.
- York A, Kingsbury S. The Choice and Partnership Approach: A Guide to CAPA. CAMHS Network. 2009.
- Date modified: